This post includes a raw transcript and screenshots/ quotes from the March 5, 2020 media event where U.S. "Military Medical Leaders" discussed “whole of government” efforts for the development of vaccines and other “countermeasures” against Covid-19. The relevant links - for DoD and C-SPAN websites - are at the end of this post. A PDF of the transcript will be uploaded in due course. For context please see our “Countermeasures Coup” post from 15 February 2024.
“A low risk infection… even in the absence of a vaccine”
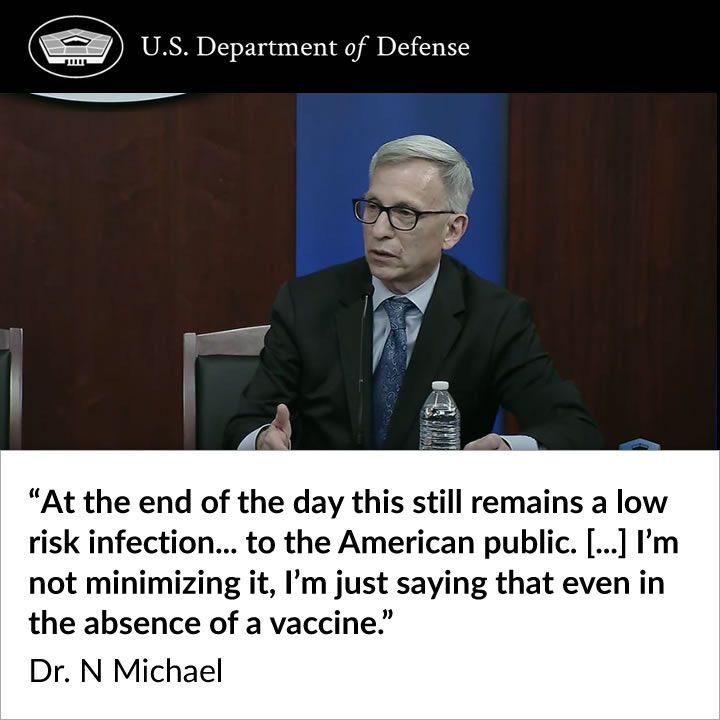
On review, the most striking moment in this elaborate piece of theater is the admission - by a top U.S military infectious disease expert - that the coronavirus…
… remains a low risk infection… to the American public… even in the absence of a vaccine.
(Or as one of JJ Couey’s fans quipped on his livestream: “It’s a low risk pandemic.”)
Likewise, the assembled experts predict that Covid-19 will be probably be seasonal (similar to influenza):
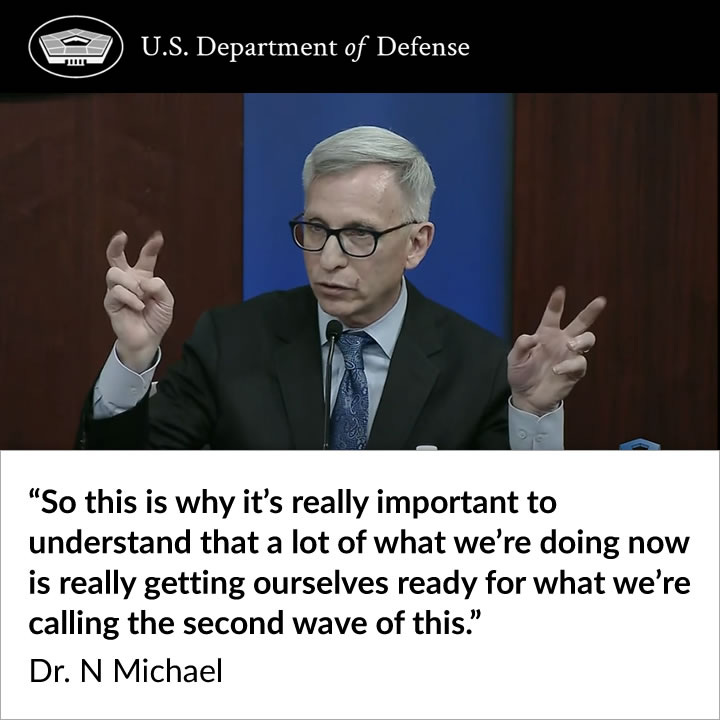
… a lot of what we're doing now is really getting ourselves ready for what we're calling the second wave of this.
(From another JJ Couey fan: “Getting ready for the second wave of money.”)
The dramatic explanations about “whole of government” and international efforts (in collaboration with existing inter-agency, industry and academic partners) regarding modelling, mass-testing and mass-vaccination to “defend the homeland” and “protect the citizens of the world” are in stark contrast to all of the above.
The press conference was five days before the WHO announced a 'pandemic' and ten days before the shock-and-awe lockdown of the United States by members of the White House Coronavirus Task Force. And it was more than two months before the start of “Operation Warp Speed”.
Interestingly, the word "pandemic" was not used once by the panel of top infectious disease doctors during the press briefing on 5 March 2020. Neither was there a reference to "pandemic preparedness" - the focus of the pre-Covid Event 201.
This performance fits perfectly with what JJ Couey refers to as “Team Worst Case Scenario”.
So: Why was there a “vaccine solution” to “protect the citizens of the world” for what was acknowledged to be “a low risk infection… even in the absence of a vaccine”?
Joining the dots… Please watch (or rewatch) this three minute video from 4 June 2019 - “Medical Rapid Response” - by the U.S. DoD’s JPEO-CBRND, outlining “Rapid Response Partnerships” between government, industry, academia and NGOs at the national and international level for the purpose of developing and deploying mass medical countermeasures - from diagnostic tests to targeted ‘vaccines’ - in the event of an ostensible biological threat.
And then listen to Brig. Gen Michael Talley’s opening statement to the media on 5 March 2020.
“Medical Rapid Response” - U.S. JPEO-CBRN Defense - 4 June 2019 - youtube
[See our “Preview” post for the transcript of the JPEO-CBRND video]
"The Covert Response"
We have included the visual of closed captioning that appears on both the Department of Defense and C-SPAN websites in reference to Dr. Deborah Birx's role - mainly because it is consistent with her own account of the part she played in “15 Days to Slow the Spread”.
Full transcript:
“Military Medical Leaders Discuss Vaccine Development Against Coronavirus” - 5 Mar 2020
Kathy Turner:
Okay. Okay. Good afternoon, everybody. Thanks for coming to our press briefing on the Army support to vaccine development. My name is Colonel Kathy Turner, I'm the director of the Army Media Relations Division and I will moderate today's session. The following senior leaders are on today's panel. We have Brigadier General Mike Talley, Commanding General of the U.S. Army Medical Research and Development Command and Fort Detrick. We have Colonel Wendy Sammons-Jackson, Director of Military Infectious Diseases Research Program U.S. Army Medical Research and Development Command. We have Dr. Nelson Michael, Director of the Center for Infectious Disease Research, Walter Reed Army Institute of Research. And we have Dr. Kayvon Modjarrad, Director of Emerging Infectious Diseases, Walter Reed Army Institute of Research.
Today's discussion is on the record. After Brigadier General Talley's opening remarks, I ask that you limit yourselves to one question and one follow-up until we have gotten around the room and then we'll continue to field questions until we are out of time. We have about 30 minutes today.
With that, I'll turn it over to you, sir.
Michael J Talley:
Okay. Hey, good afternoon and thank you for participating in today's briefing. Our hearts go out to those that are affected or know someone who's affected by this disease. Emerging infectious diseases like this coronavirus that we're facing now, or Covid-19, are why a global network of military infectious disease surveillance laboratories exist around the world. Military medical research is a force multiplier designed to support the service member and the public in every conceivable circumstance.
In his prepared remarks for the press briefing on 5 March 2020, Brig. Gen. Michael Talley repeatedly used the term “whole of government” to describe the Covid countermeasures plan of attack.
Through both emerging science and technological advances, the United States Army Medical Research and Development Command is on the forefront of delivering medical capabilities faster and more efficiently than ever before. We are supporting a whole of government approach to detect, prevent, and treat Covid-19 and when it comes to infectious disease threats, we have extensive capabilities and an international research infrastructure already in place that allows our scientists to anticipate and develop countermeasures against emerging infectious diseases.
Covid-19 is the infection caused by the SARS-CoV-2 virus, and this is familiar territory for our team. Our labs have previously studied SARS and MERS, both of which are coronaviruses; they're in that same family. Our researchers and scientists at the Walter Reed Army Institute of Research conducted the first in-human phase one trials of the MERS vaccine, and that's the only MERS countermeasure and only the third coronavirus vaccine ever tested in humans.We're building upon the science for Covid-19 solutions as we speak right now. Just this week, we were able to develop new versions of Covid-19 candidate, one of the first candidates that we've tried, and we initiated research to determine if there is a response to the vaccine. Again, this is just one piece of the solution. There's other vaccine candidates being developed by other organizations, but we're all working toward a solution and we want to get it done as quickly as possible and we're doing this in a whole of government fashion and certainly a whole of DoD fashion.
In addition to vaccine prevention, we are also exploring treatments. Efforts are ongoing right now to identify new drug candidates to respond to the Covid-19 infection. A cooperative research and development agreement with an industry partner is under review for the DoD to gain access to an antiviral drug for treatment use in our medical centers, our military treatment facilities. Together with our United States government partners, we are progressing at very fast rates, revolutionary rates almost, constant effort, and this is in order to deliver effective treatment and prevention products, products that'll protect the citizens of the world and preserve the readiness and lethality of our DoD's service members.
I want to thank you in advance, but I'd also like to tell you a little bit about my teammates here. So Colonel Dr. Wendy Sammons-Jackson is the Director for Military Infectious Disease Portfolio. She dual hats as the Joint Program Committee Director for the entire DoD. So when you're looking at the capabilities and capacity within the Medical Research and Development Command, the demand signal is coming from all over the Joint Forces. She's managed that portfolio for the last two years and when you talk about some of the most recent accomplishments with MERS, with Zika, she has been involved in all of those things.
Dr. Nelson Michael, about 37 years of experience. Same thing, we talk about some of our latest successes with MERS, both he and Dr. Kayvon Modjarrad have been right at the forefront. Even with Zika, very proud to say that within nine months, this is the team that was able to start the first in-human clinical trials. Just last December of '19, the MERS-CoV, (correction) the Ebola Zaire version vaccine was given full FDA approval. These two gentlemen played a big part of that.
Dr. Kayvon Modjarrad, again, having been the scientist behind a patented adjuvant that's designed for this same family of diseases, it's an adjuvant that's being used right now, being shared with our whole of government partners. He just recently returned from Switzerland. We were lucky enough to be able to recruit him from the World Health Organization and he's been back for about a week from Switzerland.
When you look at certainly the scientists that we recruit and train within the DoD, they're well integrated with some of the top scientists in the country, and so we're very proud to take part in this effort and we look forward to your questions.
Kathy Turner:
Okay. Lolita?
Reporter 1:
I'm Lolita Baldor with the Associated Press. For whoever this most applies, just on the vaccine, can you talk a little bit just more detail about the vaccine, your work that's being worked on? Is it different than NIH's approach and how soon are you for a phase one trial? And then I'll just throw the follow-up out just in case that's easier. The rapid diagnostic that is being worked on, can you talk a little bit about that and where you are in the rapid diagnostic tool and how soon that might also be available for testing?
Michael J Talley:
Yes, ma'am.
Nelson Michael:
Let me just take the first two questions quickly and give you over to Dr. Modjarrad who can talk about some more granular aspects of this vaccine. First thing I just want you all to know is that we have been around the Walter Reed Army Institute of Research for 127 years. I mean, a lot of people like to ask, "Well, why is the Army involved in vaccine development?" We've been doing this for an extremely long period of time. Walter Reed obviously made his notoriety on figuring out countermeasures to yellow fever. So we've been doing this for an extremely long time, one. Two is that we work very closely in the interagency space. My first rater in the army, recently retired, is Rob Redfield as the CDC director. My second rater is Debbie Birx, now obviously the Global AIDS Coordinator and running the Covid response under the Vice President. Dr. Fauci is close enough to him that he retired me about 18 months ago.
Dr. Nelson Michael said his “second rater” in the Army, Dr. Debbie Birx, was now running the covert response under the VP!
(See closed captions on DoD and C-SPAN websites from 08:20 onwards)
So we work very, very closely in the interagency space in the vaccine that I'll let Dr. Modjarrad talk about, we worked with Dr. Fauci's team to find a space where we could find a vaccine candidate that was scientifically not duplicative, but mutually supportive of what others were doing, but also made sense and so we ended up moving on two different vaccine platforms in coordination with Dr. Fauci and his team. Let me let Dr. Modjarrad tell you a little bit more about that and what our rough timelines could be.
Kayvon Modjarrad:
Thanks for your question. So from the first day that the sequences of the new virus were published, we were working on this vaccine and we were doing so in coordination with our interagency partners at the NIH, specifically the Vaccine Research Center where the President was visiting just a couple of days ago, which is a place that I came from where I trained under Dr. John Mascola and Dr. Barney Graham there and have been in constant communication, very much like we did for the Zika vaccine where the NIH and Walter Reed Army Institute of Research had two complementary approaches towards a vaccine candidate for Zika.
Here, again, we're taking a platform that actually has been used in clinical trials so far for influenza, a different respiratory virus, and focusing on a component of the virus that a lot of groups are working on, but with a unique platform and a unique what's called adjuvant, which is a chemical that is used in combination with vaccines all the time to enhance their immune response. That adjuvant is actually patented by the army. So we see this as a unique and complementary approach that is non-duplicative, that is being coordinated as part of the whole of government response.
Nelson Michael:
I know you asked the question about the point of care testing. Unfortunately... I think we have the world's leading expert in infectious disease diagnostics, who just happens to be in the army at the Walter Reed Army Institute of Research, Dr. Sheila Peel. Sheila, like me really, has been working on HIV almost her whole professional career and there isn't a single HIV rapid test that's out in the market that hasn't at some level passed through her hands. So she's really our lead for looking at the diagnostics that are currently being used, a test that would allow us to understand whether someone's infected or has been exposed. And I can tell you that for now, most of those tests are based on detecting the virus itself.
So developing the kind of test like a pregnancy test that you might be familiar with is requiring a different kind of technology. Sheila is already having those kinds of discussions. I think what you're going to probably see is much more sophisticated and higher throughput tests that initially will be done in more sophisticated laboratories and then as time goes on, that technology will then roll out to establish platforms to allow these tests to be moved more at the point of care.
Reporter 1:
But, I mean, do you have a sense on when you'll have a test ready to roll out? Do you have a sense of any timing on that? And do you have a sense on whether this vaccine, when that would be? Have you started testing in animals or the phase one trial? Do you have timings?
Nelson Michael:
Okay. As far as the diagnostics are concerned, there are large and very competent commercial concerns that are looking literally in the next month or two, to convert the current assays that are really relatively slow to execute and can only do a small number of samples at a time to being able to do these on very robust machines that could execute up to 800 tests per eight hours, which is a standard work shift. So those are the kinds of approaches that the industry has already done. I mean, we do HIV testing, we do almost a million HIV tests a year at our laboratory up in Silver Spring, and we use those kinds of instruments, so they can be adapted for those kinds of other technologies. Let me let Dr. Modjarrad talk about where we are in terms of stages of development, pre-clinically then into the clinic for a vaccine.
Kayvon Modjarrad:
So if we think about vaccine development at different stages, the first stage is the design and the discovery to decide what is going to be your candidate. We've completed that and we have gone into small animals, mice. So we're looking at what the response is to that vaccine in mice. And then as far as a timeline to getting into humans, I wouldn't want to speculate too much on that. I think the important thing to consider also is that going beyond a phase one study, there's the second phase, which is often times looking in a larger population at the safety and the immune response, but also then transitioning to see if it's effective in populations. What I think the field is trying to do is position itself as a whole so that if there's a second wave during the next season in the winter, that those candidates have made it through phase one studies to be ready to look at the effectiveness during the next season.
The anticipated “second wave” and seasonal pattern of Covid-19 was outlined by Dr. Kayvon Modjarrad and colleagues.
Kathy Turner:
Okay, so let's go to Caitlin and we'll come over to Tara. Caitlin.
Reporter 2:
It's a question/ request. With describing the vaccine, can you be a little bit more broken down in terms of language about what you're talking about? Because you're talking about candidates, which... What does that mean? What does it mean for vaccine platforms? Just so that we can communicate best about what you're kind of really talking about.
Kayvon Modjarrad:
Yeah. Thank you. So think of this as the virus. My fist, it's a sphere, right? And it's got little spokes coming off of it that makes it the corona. When you look at it on cross section, it's got that crown look to it. So almost all the vaccine candidates out there are focused on that little spoke, what we call the spike, the spike protein, and there are different parts of the spike that mediate the attachment of the virus and the entry of the virus into our cells in our lungs. So if you block that attachment, if you give a vaccine that trains and educates your immune response, your immune system to recognize that part of the virus that attaches to your cells and blocks it, that's going to be a good vaccine. So that's why everybody's focused on that. And then so what's a candidate then? Candidate means that you're looking at options.
You got your different options, that's your different candidates, and you look in mice or other animals. Other people are looking at other animals as well as our scientists are doing within our command to see which of those options looks best in small animals and then large animals before you go into humans. As far as a platform, so you have that little piece of the virus that is going to be the part that educates your immune response, but you need to deliver it in something to the body.
You need to get it expressed in your body, and there are different ways to do that. You can have it on a nanoparticle, basically something, another sphere that kind of looks like the virus. You can have it in DNA, which is part of the same kind of DNA, but it goes into our body and our cells express that. The Moderna vaccine that you've probably heard about in collaboration with the NIH, that's mRNA. It's a different kind of thing like DNA. That's the platform parts, the part that expresses that candidate that we're trying to find out how good it is in different animals. Hope that helps.
Kathy Turner:
Thank you for asking that question, Caitlin. We are going to go to Tara and then we'll head back over to Phil.
Reporter 3:
I'll say thank you too. I was about to ask something kind of related, but tied to that, could you talk a little bit about what your scientists are actually doing in the labs? Are they working with test tubes? Did they actually get samples of coronavirus from someone who was infected? How did they do this?
Wendy Sammons-Jackson:
Happy to. So our scientists are doing a number of things right now. There has been receipt of the virus in one of our laboratories, and they're currently culturing, growing that virus so that we can have stocks available for a number of things to test products with. They're also doing characterization of the virus to try to understand, learn more of what we know about the virus and how the virus impacts the host and our immune response to that virus. The scientists and our other support laboratories are... Yes, test tubes, pipettes, they're dealing with mice, they're running cell cultures, and I can let the scientists here that are doing the hands-on work talk a little bit more.
Michael J Talley:
One description in the laboratory that received the samples that Colonel Sammons-Jackson is talking about is the US Army Medical Research Institute of Infectious Diseases at Fort Dietrich. But if you think of the movie "Outbreak" and the suits that they wore and the highly contagious environment without all of the drama of the movie, certainly, but that capability certainly exists within military medicine. And that particular laboratory is the DoD's only biosafety level 4 laboratory. So that type of work, and we're not there yet with coronavirus where we would actually bring it into containment facilities or laboratory suites to test it at higher levels. We mentioned small animals that would be an advancement to a larger specimen, perhaps, not there yet, but that's what the laboratory work looks like. And I think we're actually conducting that to some degree now in BSL-3 conditions. Biosafety level two conditions. But to get a picture of what that looks like at low scale levels in vitro, under microscopes to all the way to where we would actually begin advanced types of testing there. That's where we're skating through, if you will.
Wendy Sammons-Jackson:
MRDC, Medical Research Development Command is really fortunate because we have a very unique national asset as the General mentioned in our institute for biosafety level 3, which is current virus is required to be handled within as well as biosafety level 4. And so those scientists a critical asset and those scientists are actively working to investigate the virus as well. In addition, we also have the Walter Reed Army Institute of Research with our two scientists here over here who are working in biosafety level 2 and doing the discovery, the small animal work, and have some of the most brilliant minds in the world working in infectious disease research. And so within that, we have a very robust science and technology platform. In addition, we also have the capabilities to take products from the science from the prototype level and move them into advanced development, which is required in order for us to move them into manufacturing and commercialization. So within MRDC as a whole, we have sort of the entire pipeline for developing products.
The Medical Research Development Command (MRDC) had “the entire pipeline for developing products” as explained by Col. Dr. Wendy Sammons-Jackson
Reporter 3:
And just super quick follow up, where did the sample come from? The coronavirus sample you're working on.
Wendy Sammons-Jackson:
The CDC.
Reporter 3:
Okay. But isn't there a geographic area that can be identified of where the infection was. Did it come from China or?
Kayvon Modjarrad:
It came from a US patient.
Nelson Michael:
Yeah, I think it was Washington State, but yeah, [-] it's domestic.
Kathy Turner:
Okay, so let's get some more questions in here. So let's go to Phil.
Reporter 4:
So just to clarify really quick on the rapid diagnostic that Lolita asked about. What, first of all, you said, I thought it was clear, you said it'd be about a month or two months before you think such a diagnostic would exist?
Nelson Michael:
No, no. I was saying that industry right now is taking their very robust platforms they have been using for a long time to do high throughput screening for other infectious diseases and are adapting those for the testing for the SARS coronavirus 2. The point of care tests, if they're going to be actually detecting the virus itself, that's a lot trickier to actually take that kind of technology and then making it really small. So I will tell you that we ourselves are not involved directly in those efforts. We're becoming aware of those that are, because historically we've made so many kinds of research projects along with industry to advance point of care tests largely for infections like HIV because we're heavily involved in the President's Emergency Plan for AIDS Relief, which obviously the point of care there are places that are resource constrained in Africa largely.
And so you really need those kinds of robust tests that require very, very little skill. I could probably teach my cat to use one. That's the sort of test you want to be able to use in the field. It's the same mindset we use in the military to be able to have those in rucksacks, right? So that technology, I don't want to leave you the impression that that's going to be available anytime soon. Clearly we're focused on is the more complex laboratories so that we don't have state and local departments of public health that are simply overwhelmed with individuals that want to get tested. So in those situations where the patients are coming to a central place, there having the high throughput test make sense. If now you're talking about distributing people that want to go detect in less dense populations, that's where the rapid or point of care tests will be important.
Reporter 4:
Are you preparing yourselves for the possibility that the military is going to have to test military patients? I mean it's a very large community, and when you think about all the people around the world, it's unlikely that the civilian capacity would necessarily be there for everyone as fast as they need it.
Wendy Sammons-Jackson:
Absolutely.
Reporter 4:
What does that look like? I mean, right now my understanding is there's only a small number of kits that have been distributed to a very specialized, about a dozen or so labs. So what does that look like when you're talking about getting ready for testing over a million people, maybe potentially in the US military?
Wendy Sammons-Jackson:
So the goal... And there's multiple approaches. So the goal is just increase capacity. And as Dr. Michael mentioned, one way to do that is to develop these high throughput assays and place them in regional, critically strategic regional areas so that we can increase the throughput of the diagnosis. Another approach, as was mentioned before with the point of care, is actually reaching further out into the environment to be able to test and rapidly as an initial screen for folks to kind of help understand what the epidemiology is. And so there's multiple approaches within the army, across the DoD and across the US government as well. Certainly critical. And each one of those approaches is our industry partners in this to be able to take a product, develop it, and commercialize it. So we are working with a number of partners and providing the support within the laboratory to help develop those capabilities.
Kathy Turner:
So let's go to Lucas and then we'll hit Courtney in back.
Reporter 5:
Lucas Tomlinson, Fox News. In your modeling, how many US military service members do you think are going contract the coronavirus?
Michael J Talley:
That'd be speculative, sir. I don't think we have done any estimates on that. It would depend on the spread, certainly the way it's progressing now, but right now we don't have data.
Screen shot of U.S. “Military Medical Leaders” at the Pentagon press briefing on 5 March 2020
Nelson Michael:
Well, I think the General's a hundred percent right. We don't have any data right now, but we're beginning to work with partners that Dr. Modjarrad can get a little bit more into that. There are lots of people now that have gotten pretty sophisticated by trying to model infectious disease outbreaks. You know, regrettably, because one seems to come every year or so, we're getting very good at this. The problem with the models, it's as only as good as the data you have that would build into it, right? So I would just say that we're beginning to set ourselves up with really good modeling groups to be able to ask questions in areas of the world where the virus is already spreading very quickly and we have good epidemiology data that would allow us to inform those models. That's going to give us some prediction.
But I can tell you during the Ebola outbreak, I literally sat in a WHO meeting and had one modeler talk about when the epidemic in Liberia was going to peak. And essentially I looked at the numbers, I said, "You're basically saying that it's only going to peak when every single human being in Liberia is infected?" And he basically just shrugged. So you just need to be careful that these models sometimes can really look bombastic. And they're only as good as the data that initially goes into them.
Michael J Talley:
One thing I can say is that the current assay, which is a test, I think the throughput is around 60 patients every eight hours. So when we're looking at volumes or what we are trying to develop in the area of detection, our goal is anywhere from 275 to 500 every eight hours. So if we can increase the throughput for this, when you're talking about a large number that would be affected, take the military for example, we're certainly developing things in case that were to happen. That goes for any population.
Kathy Turner:
Okay. So I want to go-
Reporter 5:
I think the doctor was going to say something.
Kathy Turner:
Go ahead.
Kayvon Modjarrad:
I would just add, so I think General Talley is correct and that any kind of numbers, specifically numbers you throw out there, is speculative. However, we have epidemiologists at our institute working with others - modelers - who do this all the time in the Defense Threats Reduction Agency, DTRA, who provide responses to the requests of all the different geographic combatant commands. And we have been working with them for the past few weeks initially based on assumptions, but now more importantly, on real-life data. So we're trying to refine those models better based on the data that we feed into them. So this is something that we're working on, but I wouldn't speculate and give you specific numbers.
Reporter 5:
Just one small follow-up. What is the earliest that a vaccine would be ready for a US military service member?
Kayvon Modjarrad:
So again, it depends on what you're talking about in terms of ready. So as I said, when we go into phase one clinical trials that we have done in the past, the volunteers who are involved in those trials are a mix of civilian and active-duty populations. And then as you go further on, there is in discussions with our partners and our military treatment facilities, the potential to have them involved in clinical trials. As far as licensure, whether you're talking about emergency use authorization or full licensure, if you talk about vaccines in general, I think Dr. Fauci's remarks that he's stated over and over again are really the benchmark that we should use as the most accurate, as being the earliest, earliest, earliest, probably 12 to 18 months to get something out to the population. And that would be whether it'd be civilian or military population.
Nelson Michael:
And just recognize that part of that hesitation, I mean, the science can go very quickly, but you at first don't want to do harm, right? And there obviously vaccines that can cause harm, and they provide benefits. So that mixture is something you always have to look at. And so part of the hesitation to say, oh, we can get a vaccine quickly, is you need to make sure that it's really safe. If you test a vaccine in 1,000, but one in 10,000 people is going to have something terrible that happens until you get to those numbers, you may end up doing mass vaccination campaigns with a vaccine that could cause a significant amount of problems. So this needs to be a constant reassessment of the risk and the benefit.
The other thing I would tell you, and this is a really good benchmark. We were the first people that tested the vaccine that eventually got licensed by Merck for Ebola. That vaccine was first tested by the Walter Reed Army Institute of Research. Five years later it was approved by the US FDA. In the meantime, a half a million souls were vaccinated with it, largely in Africa, especially during the outbreak in the Democratic Republic of Congo. So, you know, again, that was a risk/benefit assessment. The leadership in the DRC said, "Okay, we know it's not approved yet by European Medicines or by the US FDA, but we have a terrible outbreak of Ebola, which is highly fatal." And so decisions were made to use that under emergency use authorizations. And so there's always that kind of debate, but I think that's a good benchmark for vaccines.
Let me also say that we haven't really talked much about this. We are beginning to make other countermeasures. One of those are monoclonal antibodies. So antibodies are part of our immune response. That's part of the way the body tries to push infections back, but we can actually make these in test tubes. And these are becoming a much more common tool that are being used, especially in the fields of oncology, but increasingly in infectious disease. So instead of actually waiting for a vaccine to be made, giving you that vaccine and waiting the time it takes for it to develop the immune response, you can give, with these kinds of reagents, you can give almost immediate protection. So we're literally in the process now of beginning to take those first baby steps.
As well as looking at, we talked about one drug, the General talked about that one drug that's currently being repurposed and has been looked at for Ebola and now is being looked at for CoV-2. But there are other small molecules that could be discovered. And one capability that we have at our institute is -- every malaria drug that's ever been discovered is at some level gone through the Walter Reed Army Institute of Research. So we have a really good drug discovery program, and so we're looking for other kinds of drugs that might be lead candidates in partnerships with the pharmaceutical industry that we could bring those to bear. So vaccines, monoclonal antibodies and small molecules, "drugs", that could be brought to bear. So we don't have one theme in play. We have actually a number of things in play. And all of these are being coordinated very closely with our partners, either in government or in academia or in industry.
Kathy Turner:
Thank you, sir. I want to try to get a little bit more questions out there. So Courtney, we'll go to you.
Reporter 6:
Courtney Kube, to you with NBC News. I want to ask a couple of clarifications. So when you're saying that there's testing going on in mice, Dr. Modjarrad, you mean you're not saying that they're being injected with the coronavirus and that... right? Okay. I just wanted to be sure of that.
Kayvon Modjarrad:
Just injected with the vaccine candidates, those options.
Reporter 6:
To see how the body...
Kayvon Modjarrad:
To see how the immune response... yeah, to see how it responds to the vaccine, not the virus.
Reporter 6:
Okay, good. I just wanted to be sure of that. And then I was a little unclear, Dr. Michael, when you were talking about potentially rolling something out the next time, the next season, which I would assume would be fall, winter, or maybe it was you, Dr. Modjarrad, forgive me, the next season, but I don't quite understand what that was you were hoping of rolling out?
Nelson Michael:
Okay, so that's a really important question too. Was there a third?
Reporter 6:
The third one was just about the production, but keep going.
Kathy Turner:
Keeping it two. Keeping it two.
Reporter 6:
Yeah, I think you kind of answered the other one. So if we could do those two, that'd be great.
Nelson Michael:
So this is a respiratory virus and they always give us trouble during cold weather for obvious reasons, we're all inside and windows are closed, etc. So we typically call that the influenza or the flu season. So our expectations that this virus, like every respiratory virus, is going to be less troublesome for us as the weather warms up. And that's going to be true across the globe. But our experience, and most of our experience comes from influenza, which is unfortunately the king of respiratory viruses, but we know a lot about that. And our experience there is that every flu season equals, you know, when the weather gets cold again, this is when these viruses tend to come back.
So this is why it's really important to understand that a lot of what we're doing now is really getting ourselves ready for what we're calling the second wave of this. We hope that that doesn't happen. If you remember SARS, SARS came and went very quickly, and I really hope that happens again, but we can't count on that. We have to be ready that even if this epidemic begins to wane, we have to be ready for next winter when it may come back again.
“SARS came and went very quickly, and I really hope that happens again, but we can't count on that… we have to be ready for next winter when it may come back again” explained Dr. Nelson Michael.
Reporter 6:
I'm sorry, I still don't understand what it was that you were hoping to roll out with the next wave?
Nelson Michael:
Oh, so we're saying that as we begin to develop any of these countermeasures we're talking about, monoclonal antibodies, drugs, vaccines, that even if this disease abates over the next few months, we're very concerned that it will come back and it may come back again in the next flu season. If that's the case, then in the meantime, we've been working steadily on these countermeasures so that they'll be ready if there's a next time.
Reporter 6:
Thank you.
Kathy Turner:
Okay, so let's get [-].
Reporter 7:
Thank you. I also just have a couple clarifications, so hopefully this will go quick, but following up with her, just to reiterate, so you're testing in small animals, mice, now you're testing the candidate. And then you had said something about the second phase was looking at large populations of mice, would that be, I mean large populations of mice, or would that be of something else that you said that thinking about this next phase in the winter? I'm not quite sure what's going on?
Kayvon Modjarrad:
So I'm just going to break it down again in terms of what are the general phases of vaccine development. First you decide down at the atomic level what your vaccine is going to be. And then you have your best guess, and you have a few different options as to what that will be. Then you test all those different options in mice, meaning testing, give them the vaccine and see what kind of immune response they have. Then, typically you go into larger animals, like monkeys, right? That's typically the case. This is a new virus. We don't know which one of these animals is the most relevant one to humans. Mice are mice. Mice are not humans. Monkeys may be a little closer to humans. And then you go into humans, and when you go into humans in that first phase, you're just again, looking at the safety of your vaccine and the immune response. You're not looking at if it's effective to protect you from the virus.
The next phase is where you look at larger numbers of people for safety and immune response, again, because the first phase in humans is just a few dozen people. Now we're talking hundreds to thousands. And you start looking at: Is it protecting against infection? And you need to have large numbers of infections going on to be able to know whether or not it's protecting against that. So that's why we anticipate potentially if there's a second wave, we got to be ready, make it all the way through those first studies and the animals and the safety and the immune response so we're ready and positioned and ready to go if this comes back and there are a bunch of infections, so we can know: is it protecting?
Reporter 7:
Okay, so you're planning to be at that second phase of humans by next winter, just that's where you are? Okay. Just wanted to clarify that. And then the other thing I wanted to clarify is you said you had a candidate that was complementary but not duplicative. What exactly is the candidate? I know you talked about the spokes. Are you two focusing on the spoke of the virus?
Kayvon Modjarrad:
Yes, we are.
Nelson Michael:
Yes.
Reporter 7:
But that's just what NIH is also working on. So everybody's working on the spoke right now, just different?
Kayvon Modjarrad:
Different ways, different parts of the spoke or different versions of it, and then different ways to express it. So as I said, there's different ways. So there's a DNA platform, we can express it. There's the mRNA that Moderna is doing with the NIH. They are just using the protein itself, that's putting it on a nanoparticle protein. So there's different versions of the vaccine and different ways to present it to the immune system.
Kathy Turner:
Okay. So I know we're at 10 after right now, so we'll hit Haley and we're probably going to wrap it up. So Haley, go ahead.
Reporter 8:
Thank you. And thank you all for doing this. One question for you, General Talley. Last year in the fall, Fort Detrick, the research institute, had to pause testing for some safety concerns. Can you go into what has been done since then, just sort of make that a non-issue? And then is also, I know that [Rare] has gone over, you said different SARS and different strains of this. What makes this different from the previous strains that you've been looking at and how have you noticed those differences and how that will affect the vaccine that you're developing?
Michael J Talley:
Yeah, absolutely. I appreciate the question. Yes. So United States Army Medical Research Institute of Infectious Diseases, and that's the BSL-4, Biosafety Level 4 lab that I mentioned. But on the 18th of July of 2019, they were issued a cease and desist order by the CDC, violations because of improper practices, all resulting from a number of structural defects. They developed workarounds that just were not safe. There was never any danger of risk to the community or breaking the containment, which is what the labs are for.
Since then, proud to say, worked very hard to come back and meet CDC regulatory standards. The CDC came back for a re-inspection after about a 90-day plan of action and milestones, very aggressively went after that. And the CDC restored the laboratory to a limited operational capability, limited in that the same volume that the laboratory had become accustomed to throughputting, much smaller levels. And then certain types of testing, as I mentioned, BSL-4 being the highest type, Biosafety Laboratory 4 being the highest level, not to that level, but probably a smaller level or a level just shy of that, where the most dangerous procedures weren't being done. This was in an effort to begin a gradual standup of capabilities after being down for so long.
The CDC came back two weeks ago, first two weeks, actually three weeks ago now in February, came back for a second inspection. This inspection was to allow even more capabilities, more capacity, to be performed. Again, proud to say, night and day difference according to the CDC. And we were issued a letter to restore even higher level capabilities. That letter was issued to us just this past Friday. And so with respect to coronavirus, and coronavirus is not considered a safety level type of virus that falls into the same category as some of the other higher types. So we have full authorization to perform at the highest levels of scientific capacity at the laboratory for coronavirus. Other types of diseases that might meet some of the CDC's criteria, still having a gradual return to full operations. But with coronavirus, we are going to be able to conduct laboratory research at the highest levels that the laboratory can perform.
So that's where we are, real proud. It's been a work in progress. We took advantage of the operational pause, if you will, to really refine our standard operating procedures. And frankly, the complete culture has changed at that institution and they're back. And certainly with coronavirus, it's amazing to watch the entire enterprise mobilize the way they have. Thank you.
Kathy Turner:
Okay, so she had a follow-up first on SARS.
Kayvon Modjarrad:
So regarding your second question about how this virus differs from others and what we've learned, probably everybody's familiar now of some of the... That there are seven human coronaviruses that we know of and that the highly pathogenic ones, the ones that tend to kill, are SARS-1, Middle East Respiratory Syndrome coronavirus, and then the current coronavirus. And so we have been working on those other very more dangerous and deadly viruses like MERS and the first SARS. What we've learned is really at the very basic atomic level. When I mentioned that we first look at the atomic level of these spokes, these spikes, that's where we've been focusing on because that's where the differences matter the most in terms of what kind of immune response you get to it, how efficiently it attaches to the cells in your lung.
And one of our chief scientists, Dr. Gordon Joyce, has been doing a lot of the work on that in determining the structures, in collaboration, again, with our partners at the NIH, National Institutes of Health, the Vaccine Research Center. So Dr. Joyce, myself, we both came from the Vaccine Research Center, working with Dr. Graham and Dr. Kizzmekia Corbett, under Dr. John Mascola. And then one of the other structures that came out is Dr. Jason McLellan at the University of Texas at Austin. This should give you an idea also how this is a very tight-knit family. We're spread across different centers, but we talk to each other all the time because we have that very close public health and scientific community.
So there are similarities between this virus and some of these other viruses, but there are obviously very key differences. Between MERS and this SARS-CoV-2 there's about 50% difference in the sequence. With SARS-1, there's about 20% difference, but that 20% matters obviously quite a bit. And so that's the kind of studying that we've been doing. When we first got those sequences and the world got those sequences back on January 10th, we started looking down at the atomic level as to how they differ.
Kathy Turner:
So ladies and gentlemen, I know we've been going for a little bit, so I want to be able to wrap this up. Sir, we're going to have folks standing by to do the follow on questions, but sir, if you want to do closing remarks.
Reporter 3:
Just one last before... Since there won't be a vaccine ready in time for this cycle of coronavirus, could you please give your best advice to the Force and the public in general about how to kind of ride this out for now?
Nelson Michael:
Well, it really is. We are literally living in influenza season. People are getting infected and dying of this disease. I like to remind people that during the Ebola outbreak, both the one that just happened in the Democratic Republic of Congo and in West Africa, somewhere between 16,000 to 19,000 people were still dying every week of HIV infection. So, you know, the public, the medical communities, governments, we've really gotten very good at managing how we deal with the scourges of infectious disease.
So like any respiratory virus, you know, we're going to be getting ourselves into the habit of washing our hands much more frequently. If there's one thing that you can do, it's wash your hands much more frequently. So we're both clinicians as well. And you go into the hospital, a nurse will rap you on the knuckles if you don't wash your hands coming into the room or coming out even if you don't touch anything. So that's critical.
The things that we already know how to do, we do social distancing, we're not going to be doing a lot of hugging and kissing. If people are sick, they should stay home. If they really are very, very ill, then they can go into the hospital. But hospitals now are getting very good about how they would approach making sure that they can protect their staff as well as protecting other patients from someone who might be at risk.
So I think people should recognize at the end of the day, this still remains a low risk infection to not just our service members but to the American public, and that we are really good as a hospital system, as a medical care system, from both the EMT up to intensive care units, at taking care of these. I'm not minimizing it, I'm just saying that even in the absence of a vaccine. We still don't have a vaccine for HIV infection. But we have very good drugs and we're beginning to develop monoclonal antibodies.
After reassuring Americans that the infection was low risk even without a vaccine, Dr Nelson Michael said the DoD would “continue to campaign against these infectious disease threats as we would against enemies against the homeland”.
Nelson Michael:
So we will continue to campaign against these infectious disease threats as we would against enemies against the homeland. And we're good at doing those sorts of things, but the American public should be reassured that this is a threat that we're used to from the standpoint of influenza. We are working on developing measures, but everyone can assist just by washing their hands.
Michael J Talley:
Absolutely. Well, hopefully you've been able to hear that when you're talking to the different agencies that are out there and you're getting different responses for what they're doing individually. This is truly a whole-of-government approach. So certainly if one agency, one organization, if it's an industry partner, if it's academia, I think we're well nested and we're sharing information and collaborating so that we're able to leverage the right resources to bring a vaccination, or a vaccine candidate as we've learned about today, across the finish line.
So we're going to continue to collaborate in the fashion that we have, and we're going to work as hard as we can to find the right treatments, the right preventative measures, and certainly the right detection capabilities that are out there. Those are our three focus areas within the DoD. We really appreciate your time today, and again, thank you very much. It's been a pleasure. Thank you.
Kathy Turner:
So everybody, thanks for coming today. So we have some folks who are going to stand by in this room to do follow-up questions for you. Lori Salvatore from the lab is here with her team. And then we also got my team here from off the deck that can help facilitate follow-on questions that we didn't get to that you want for your reports. And then I just want to thank General Talley and his team for their time today. So thanks everybody.
Nelson Michael:
Okay.
Michael J Talley:
Thank you very much.
Nelson Michael:
Appreciate it.
One more time: “Our partners in government, industry and academia”... We’re all in this together!
Video links for Pentagon press briefing - 5 March 2020
Department of Defense - 5 March 2020:
“Military Medical Leaders Discuss Vaccine Development Against Coronavirus”
https://www.defense.gov/Multimedia/Videos/videoid/742071/?dvpTag=warp+speed
C-SPAN - 5 March 2020:
“U.S. Army Briefing on the Coronavirus Outbreak”
https://www.c-span.org/video/?470050-1/us-army-briefing-coronavirus-outbreak
Video link for U.S. “JPEO-CBRN Defense”- 4 June 2019
JPEO-CBRND youtube - 4 June 2019: